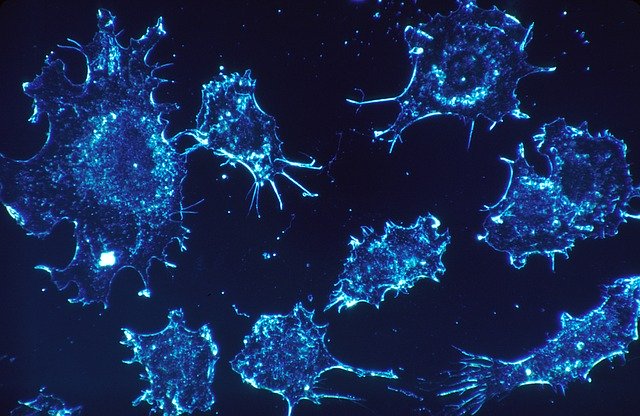
Melanoma immunotherapy is a type of treatment that uses substances to re-stimulate the immune response, which leads to the development of immune checkpoint-blocking antibodies. This form of treatment can overcome the tumour microenvironment’s inhibition of T cells. Despite its success with most patients, immunotherapy did not work for everybody. As a result, a group of researchers decided to focus their attention on identifying the mechanisms behind cancer-induced inflammation as a potential target for future novel immunotherapy.
Cancers like melanoma present with symptoms of inflammation and immunosuppressed tumour microenvironments (the structural environment around a malignant tumour). An immunosuppressed tumour microenvironment inhibits the activity of the immune system, specifically T cells, key players in the body’s immune response.
From the analysis of mouse models, tumour-associated B cells were identified to promote tumour inflammation and inhibit the above-mentioned immunotherapy responses. In 2019, Nature Communications published research focused on the effect of the tumour-associated B cells on the tumour microenvironment in melanoma and its response to immune checkpoint-blocking cancer therapy. Their research consistently demonstrated the relationship between the tumour-associated B cells from the tumour microenvironment and inflammation. When the number of tumour-associated B cells decreased, the overall inflammation and immune cell numbers also decreased.
Tumour-associated B cells can be divided into six different types
Different types of tumour-associated B cells were identified in various sections of melanoma-infected tissue. The cells were all located primarily within the margins of the tumour. Their presence indicated that melanoma cells and tumour-associated B cells had no direct communication with each other to function. The six different types were as follows:
- Activated B cell-like.
- Germinal center B cell-like.
- Memory B cell-like.
- Plasma cell-like.
- Plasmablast-like
- Transitional B cell-like.
Human melanoma protein secretions
The lack of direct communication between melanoma cells and tumour-associated B cells indicates that contact is primarily through ‘soluble’ factors. After gene and protein analysis, an upregulation of pathways associated with inflammation and immunity was shown. One of the most significantly affected pathways is the tumour necrosis factor (TNF), signalled via the Nuclear Factor Kappa B factor. This aided in B cell activation for inflammation and immune response. Simply put, melanoma cells were communicating with B cells through soluble factors by inducing a signalling pattern that in turn, activated inflammation and immune responses.
Tumour-associated B cells in melanoma express distinct functional signatures
By manually extracting specific genes from a small sample size, it was discovered that B cell types express similar functional signatures for key immunological functions. Overall, the tumour-associated B cells were shown to be able to regulate inflammation and shape the cellular composition of melanoma in the tumour microenvironment.
This study revealed that tumour-associated B cells are essential to sustain inflammatory tumour microenvironments through mechanisms unique to subpopulations of cells produced from the tumour-associated B cells. Previous B cell data was controversial and limited options for immune checkpoint blocking antibodies – an option that did not work for everybody. More careful evaluation is required, but this information may guide the development of new targeting strategies for future cancer immunotherapy.
References
- Griss, J., Bauer, W., Wagner, C. et al. B cells sustain inflammation and predict response to immune checkpoint blockade in human melanoma. Nat Commun 10, 4186 (2019). https://doi.org/10.1038/s41467-019-12160-2
2. Lee S. What is cancer? Canadian Cancer Society. Updated 2023. Accessed May 28, 2023. https://cancer.ca/en/cancer-information/what-is-cancer.