Researchers based at the Shanghai Institute of Materia Medica report that blocking a protein called DRAK2, prevents toxic fatty acids from deploying a poison pill in insulin-producing cells of the pancreas. Not only do they demonstrate that drugs can protect these specialized cells, but they also shed light on how type 2 diabetes progresses.
Type 2 Diabetes is a Progressive Disease
Generally, Type 2 diabetes is a disease that comes with age. It develops slowly and sets in due to a mix of genetics and lifestyle. It starts off with cells of the liver, muscle and fat finding it difficult to respond to insulin cues to soak up glucose. Over time, the pancreas finds it harder to make enough insulin. In the most serious cases, the insulin making cells will die. Patients can no longer make insulin, and will need insulin injections to stay alive. The good news is, type 2 diabetes is a reversible condition. If you act before you permanently damage your pancreas, lifestyle changes can get you back to normal. So how can we delay damage to the pancreas? A new research article in Science Translational Medicine may hold the answer.
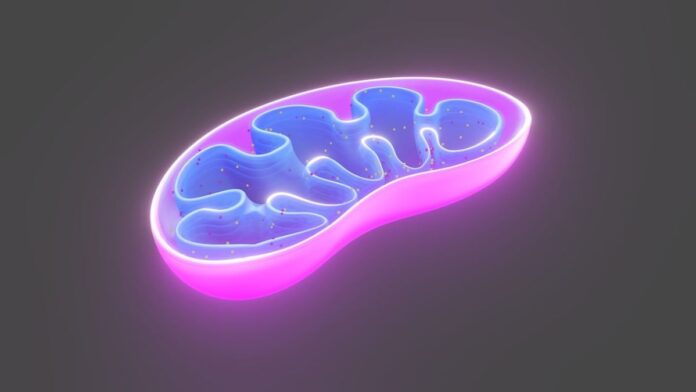
Beta cells are specialized cells in your pancreas that make insulin. They sense how much glucose is in the blood using their mitochondria. These are the tiny organelles inside your cell that we affectionately call “the powerhouse of the cell.” If there’s too much glucose in your blood, your beta cells release insulin. This tells liver, fat and muscle cells to take in the glucose and store it for later.
We can injure our beta cells in a few different ways: damage to their mitochondria, glucose overload, lipid toxicity, inflammation and cell stress. Drugs that protect beta cells from injury could buy some time for a type 2 diabetic to nurse their pancreas back to health.
Sick Mitochondria Trigger a Poison Pill in Pancreas Cells
People with Type 2 diabetes end up with sick mitochondria in their pancreas cells. The beta cells do not know how much insulin to make, because their glucose detectors don’t work.
Mitochondrial damage occurs as a result of exposure to chemical substances that damage DNA, chronic inflammation, lipid toxicity, too much glucose and aging.
Cramming mitochondria with glucose or lipids causes toxic byproducts to build up. These molecules damage the mitochondrial DNA. You can think of this as wearing out your mitochondria. Over time as we injure our mitochondria, they will be less effective at sensing glucose, and beta cells will not produce enough insulin.
The trouble is when mitochondria are very unhealthy, they trigger the cell’s self-destruct mechanism. Our cells intend this to protect us. It helps prevent cancer and it defends us against viruses. They take themselves out for the good of the whole organism. This can be very useful, but if essential cells self-destruct, it causes more problems than it solves. For example, when beta cells die, we lose the ability to regulate insulin levels.
Scientists are now working on finding drugs that can stop the mitochondria pushing the red button, and protect beta cells.
Toxic Fatty Acids kill Beta Cells
The researchers knew that poisonous fatty acids can build up and kill beta cells. They suspected that lipid toxicity might be a trigger for mitochondrial failure. They also knew that when you add toxic fatty acids to beta cells, a protein called DRAK2 somehow prompts the cells to destroy themselves.
In the past scientists had used a drug that inhibits DRAK2 to potect beta cells from dying. The Shanghai team built on this work by finding out how and why blocking DRAK2 protected the insulin secreting beta cells.
Diabetics Have More DRAK2 in Their Pancreas
They began by collecting post-mortem pancreas samples from healthy people, mice and macaque monkeys, as well as those of type 2 diabetic humans, monkeys and mice. They found that the diabetic samples had less insulin and more DRAK2. They also checked whether cells that had high levels of DRAK2 had healthy mitochondria. Mice with high DRAK2 had fewer mitochondria, and the ones they had, were sicker.
Next the researchers asked what happens if you take DRAK2 away? Could they protect the beta cells from fatty acid damage? They created a family of genetically modified (GM) mice with no gene for DRAK2 in their Pancreas. The mice were pretty normal except that in their pancreas, they could not make DRAK2 protein.
When they fed the GM mice and a group of normal mice a high-fat diet, the normal mice soon became sick. Their pancreas stopped making insulin, and they had very few mitochondria inter pancreas cells. The GM mice, however, still made insulin and had healthy beta cells with plenty of mitochondria.
An Internal Recycling Plant
Healthy cells recycle their mitochondria. When sick mitochondria send out a distress call, the cell sends it to a recycling centre (autophagosome). They can then make new mitochondria from the materials. If the cell doesn’t transport mitochondria for recyling, they send them to the trash. If the cell sends too many mitochondria to the garbage, the cell will self-destruct.
The researcher realized that when you feed a mouse a high-fat diet, eventually the they stop recycling mitochondria. When the beta cells don’t have enough healthy mitochondria, they stop making insulin and ultimately they will die. The scientists discovered that if you take away the DRAK2 protein, the cell recycles mitochondria instead of trashing them.
The researchers repeated these experiments on human pancreas cells. They treated cells with a genetically modified virus that could turn off DRAK2, and compared them to normal, healthy pancreas cells. The team fed the cells with toxic fatty acids—just like the ones your body makes when you eat too much. They showed that losing DRAK2 protected beta cells from dying, increased insulin production and happily recycled their mitochondria. The regular cells got sick.
DRAK2 intercepted the mitochondria that needed recycling, and sent them to the trash instead—triggering the cell death pathway.
DRAK2 Prevents Mitochondria From Being Recycled
DRAK2 is a labelling protein. Its normal function is to float around in the cell tagging proteins for the trash.
The team looked at all the proteins in a DRAK2 negative pancreas cell compared to a normal cell. They noticed that the protein ULK-1 was marked for trash in normal cells, but not in cells without a DRAK2 gene.This was a significant discovery, ULK-1 is a protein that the cell uses to label mitochondria to send them for recycling. Here was the link between DRAK2, mitochondria and the recycling program. DRAK2, was interfering with the recycling program by sending ULK-1 directly to the trash.
Finally, the team tested a drug that blocks DRAK2. They applied it to normal pancreatic beta cells. When they added toxic fatty acid to the cells, untreated beta cells eventually lost their mitochondria, stopped producing insulin and died.
In contrast DRAK2 inhibitor protected fatty acid treated cells. They still produced insulin and their mitochondria were working.
Drugs in Development to Protect Beta Cells?
So what does all this mean? Well, it’s early days. This research is in its infancy, but the researchers showed drugs that block the DRAK2 protein could be an excellent tool. With a bit more research and a lot more work, type 2 diabetics could keep their beta cells alive a bit longer. In an ideal world, a type 2 diabetic could take advantage of this additional time to make some healthy lifestyle changes. Type 2 diabetes is reversible.
Read the full paper here.
References
Heilbronn LK, Gan SK, Turner N, Campbell LV, Chisholm DJ. Markers of Mitochondrial Biogenesis and Metabolism Are Lower in Overweight and Obese Insulin-Resistant Subjects. The Journal of Clinical Endocrinology & Metabolism. 2007;92(4):1467-1473. doi:10.1210/jc.2006-2210
Jung HS, Chung KW, Won Kim J, et al. Loss of autophagy diminishes pancreatic beta cell mass and function with resultant hyperglycemia. Cell Metab. 2008;8(4):318-324. doi:10.1016/j.cmet.2008.08.013
Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of Mitochondria in Human Skeletal Muscle in Type 2 Diabetes. Diabetes. 2002;51(10):2944-2950. doi:10.2337/diabetes.51.10.2944
Lu Y, Xu J, Li Y, et al. DRAK2 suppresses autophagy by phosphorylating ULK1 at Ser56 to diminish pancreatic β cell function upon overnutrition. Sci Transl Med. 2024;16(733):eade8647. doi:10.1126/scitranslmed.ade8647
Maechler P, Wollheim CB. Mitochondrial function in normal and diabetic beta-cells. Nature. 2001;414(6865):807-812. doi:10.1038/414807a
Mao J, Luo H, Wu J. Drak2 overexpression results in increased beta-cell apoptosis after free fatty acid stimulation. J Cell Biochem. 2008;105(4):1073-1080. doi:10.1002/jcb.21910
Pancreatic β cell regeneration induced by clinical and preclinical agents – PMC. Accessed February 8, 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7859987/
Perl S, Kushner JA, Buchholz BA, et al. Significant Human β-Cell Turnover Is Limited to the First Three Decades of Life as Determined by in Vivo Thymidine Analog Incorporation and Radiocarbon Dating. The Journal of Clinical Endocrinology & Metabolism. 2010;95(10):E234-E239. doi:10.1210/jc.2010-0932
Song GY, Ren LP, Chen SC, et al. Similar changes in muscle lipid metabolism are induced by chronic high-fructose feeding and high-fat feeding in C57BL/J6 mice. Clinical and Experimental Pharmacology and Physiology. 2012;39(12):1011-1018. doi:10.1111/1440-1681.12017
Toledo FGS, Johannsen DL, Covington JD, et al. Impact of prolonged overfeeding on skeletal muscle mitochondria in healthy individuals. Diabetologia. 2018;61(2):466-475. doi:10.1007/s00125-017-4496-8.
Unger RH, Zhou YT. Lipotoxicity of beta-cells in obesity and in other causes of fatty acid spillover. Diabetes. 2001;50 Suppl 1:S118-121. doi:10.2337/diabetes.50.2007.s118
Unger RH. Lipotoxic Diseases. Annu Rev Med. 2002;53(1):319-336. doi:10.1146/annurev.med.53.082901.104057
Weir GC, Bonner-Weir S. Five stages of evolving beta-cell dysfunction during progression to diabetes. Diabetes. 2004;53 Suppl 3:S16-21. doi:10.2337/diabetes.53.suppl_3.s16
Wang S, Xu L, Lu YT, et al. Discovery of benzofuran-3(2H)-one derivatives as novel DRAK2 inhibitors that protect islet β-cells from apoptosis. Eur J Med Chem. 2017;130:195-208. doi:10.1016/j.ejmech.2017.02.048
Wiederkehr A, Wollheim CB. Minireview: Implication of Mitochondria in Insulin Secretion and Action. Endocrinology. 2006;147(6):2643-2649. doi:10.1210/en.2006-0057