A soon-to-be-published study supports the development of arbovirus vaccines targeting mosquito salivary proteins rather than the viruses present in their saliva.
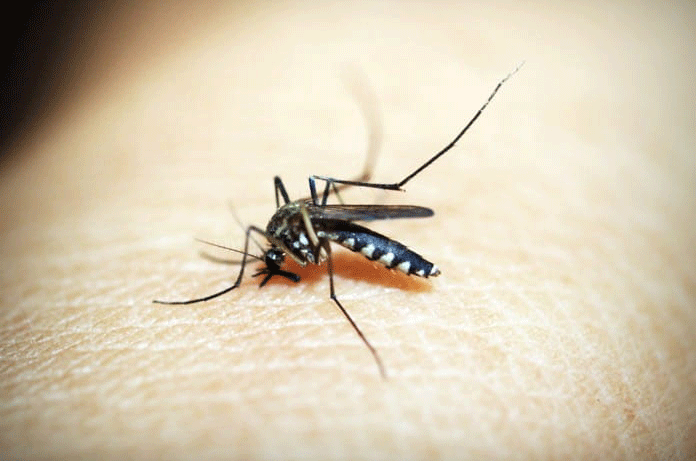
Arbovirus infections represent 17% of all communicable diseases in humans, causing one billion cases and one million deaths annually. An arbovirus is a virus that is transmitted by insects to a vertebrate host, mainly mammals. The most common vectors of the arbovirus are mosquitos, ticks, and sandflies.
The most prevalent mosquito-borne viruses are dengue, yellow fever, West Nile, Zika, and chikungunya. These viruses have been responsible for emerging and re-emerging outbreaks and epidemics in the last years, thus representing a huge global health burden. Among all vector-borne viruses, Dengue is the most clinically significant arbovirus, infecting 390 million people each year with nearly 100 million symptomatic infections.
There are currently only vaccines for three arbovirus infections
Currently, vaccines exist for only three arbovirus infections: tick-borne encephalitis, Japanese encephalitis, and yellow fever. Dengue virus vaccines have been tested, but due to the complexity within the four dengue subgroups and genetic similarities with Zika virus, further studies must be conducted.
Since the development of viral protein-based vaccines has not been successful due to the intricacies of the vector-arbovirus-host interactions, some studies have supported the use of salivary proteins to develop “universal” arbovirus vaccines.
American researchers recently conducted a review study and its manuscript will be published soon in The Journal of Infectious Diseases. In their article, the authors review the literature and encourage the research and development of such vaccines.
The role of salivary proteins in arbovirus infectivity
The insect saliva aids the infection process by promoting the infectivity of the arbovirus being carried. This means vaccination with insect saliva would regulate and direct the host’s immune response to another mosquito saliva contact, blocking transmission of disease and/or killing pathogens on the bite site. This would work as a pan-viral protection for a specific vector, like the Aedes aegypti, the vector for Dengue, Yellow Fever, Zika and Chikungunya viruses.
When a mosquito bites, it injects a mix of vasodilators, anticoagulants, and proteins with antigenic properties. These chemicals regulate and drive the host immune response towards a pathway that is not effective against viral infections, allowing the virus to spread easily and quickly. So, by interfering with the immune response that would normally fight the virus, the mosquito saliva can make the environment favorable to the survival and spread of the virus.
Some mice models have shown that the experimental injection of mosquito saliva and West Nile virus cause more severe disease than experimental injection with only the arbovirus, demonstrating the importance of salivary proteins in increasing the infectivity of an arbovirus.
Vaccines with salivary antigens
Malaria, caused by Plasmodium sp. and leishmaniasis, caused by Leishmania sp., are serious diseases that have insects as vectors but are caused by protozoa, rather than by an arbovirus. It has been observed in mouse models of these diseases that repeated host exposure to the vector saliva shifts the immune response from a non-protective pattern to a protective pattern, reducing the development and severity of such diseases.
So, it is reasonable to think that if a vertebrate is immunized with salivary proteins, a subsequent exposure to the same mosquito saliva could regulate the immune response. Because the host would have produced antibodies against saliva proteins, the protective pattern of the immune response would be maintained or enhanced, reducing the arbovirus infectivity.
What is known about other arthropods’ saliva?
The saliva of the sand fly has been extensively studied and it is known that the parasite Leishmania sp. is more effectively transmitted in naïve compared to saliva-exposed animals, due to protective saliva-antibodies produced.
Beagles and macaques immunized with sand fly salivary proteins presented a robust, long-lasting cellular immunity with a protective pattern, instead of a non-protective pattern, in visceral and cutaneous leishmaniasis infections, respectively.
Studies have also demonstrated that after repeated vector exposure, various mammalian species develop “tick immunity” that is caused by anti-salivary gland antibodies. While vaccines do exist for tick-borne encephalitis viruses, no vaccines exist for other important tick-borne diseases, such as Lyme disease, typhus, and Crimean-Congo hemorrhagic fever.
So far, human studies evaluating mosquito salivary protein-based vaccines have not been published, and some phase 1 clinical trials are taking place with healthy volunteers in non-endemic areas. Two studies in dengue-endemic areas in South America have shown that immune responses to Aedes mosquitos are short-lived without ongoing exposure to these vectors, which configures a problem for vaccine development.
However, as seen in leishmaniasis, pathogen-targeting vaccines complemented by vector salivary antigens may yield the most promising results and might be the hope for future arbovirus vaccines.
Written by Gustavo Caetano, B.Sc., M.Sc.
Reference: Manning J E, Morens D M, Kamhawi S, Valenzuela J G, Memoli M. Mosquito saliva: the hope for a universal arbovirus vaccine? The Journal of Infectious Diseases (Manuscript version) 2018.