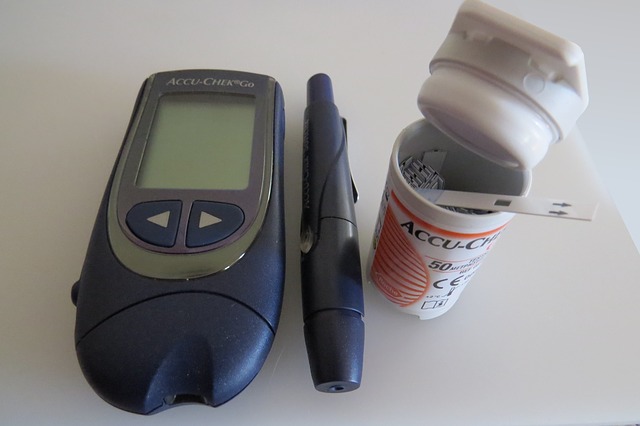
Traditional blood glucose monitors versus continuous glucose monitors – ever wondered how blood glucose monitors work?
Hyperglycemia, or high blood sugar, is a major concern in patients with type 1 and 2 diabetes.
If left unmanaged, high blood sugar can increase the risk of cardiovascular disease and induce significant nerve and kidney damage.
Additionally, hyperglycemia can also result in ketoacidosis (diabetic coma), a life-threatening emergency that can result in sudden death if it is not treated in an efficient and timely manner.
For these reasons, it is important that diabetics and other patients at risk of hyperglycemia take appropriate actions to adequately manage their sugar (glucose) levels.
To achieve this, doctors ask that patients make the appropriate lifestyle changes, including regular exercise, eating a healthy and balanced diet, and taking the appropriate medication.
They also recommend that patients make use of glucose monitors to regularly assess their sugar levels.
Traditional finger prick versus continuous glucose monitors
There are many different glucose monitors that are currently on the market, each with its own advantages and disadvantages.
For instance, traditional blood glucose monitors involve pricking the finger and using the blood to get a measure of sugar levels. These monitors, while relatively accurate, can only give a single readout at a given moment in time.
In contrast, more recently there has been an increase in the use of continuous glucose monitors, which can provide real-time, dynamic sugar monitoring over a 24-hour period.
These continuous monitors can provide a lot of additional valuable information; for instance, they can give patients an insight into how food, exercise, and other day-to-day activities may influence their glucose levels.
With this information, patients can make more informed decisions about their lifestyle habits and come up with effective strategies to manage their sugar levels.
However, the downside of using continuous glucose monitors is that they do not assess glucose directly in the patient’s blood and therefore, their accuracy needs to be validated regularly using a traditional blood glucose monitor.
How do blood glucose monitors work?
While glucose monitors can come in many forms, they ultimately work using the same principle.
Essentially, glucose reacts with the enzyme glucose oxidase to produce different chemical by-products, some of which can release electrons and generate an electrical current.
This electrical signal is detected and subsequently converted into a digital readout. The more glucose present in the sample, the more the chemical reaction will take place, and the stronger the electrical current will be.
A stronger current will, therefore, translate into a higher glucose reading. As mentioned earlier, traditional blood glucose monitors use the patient’s own blood as a sample, which can give a relatively accurate reading of blood glucose levels.
However, for each reading, a patient will need a new blood sample and this can significantly limit the number of readings a patient can get in a given day.
In contrast, continuous monitors use a tiny sensor that is inserted underneath a patient’s skin.
The sensor is coated in the glucose oxidase enzyme, which reacts with glucose in the fluid between cells called the interstitial fluid. While these monitors provide a more continuous sugar level measurement, they do not give a direct indication of blood glucose levels.
Both traditional and continuous glucose monitors provide valuable information for patients with diabetes.
They are important tools that can help patients manage their sugar levels and make appropriate lifestyle changes if necessary.
Written by Haisam Shah
References:
- National Institute of Diabetes and Digestive and Kidney Diseases
- John Mastrototaro. The MiniMed Continuous Glucose Monitoring System
- HealthLinkBC
Image by Vicki Nunn from Pixabay